The Most Human Way to Heal
Amniox is now BioTissue Surgical!

Our future journey is to bring strength to our organization, leaning on our unique pioneering heritage by bringing together BioTissue and Amniox, one company with one purpose and one vision. A single unified brand combining the unique power of both businesses. BioTissue Surgical better reflects our vision as the regenerative medicine pioneer and our goals for the future as a biologic’s provider to realize the full potential of regenerative therapy.
We are BioTissue. The most human form of healing.
Meeting The Clinical and Economic Challenge of Complex Wound Healing
The BioTissue Difference
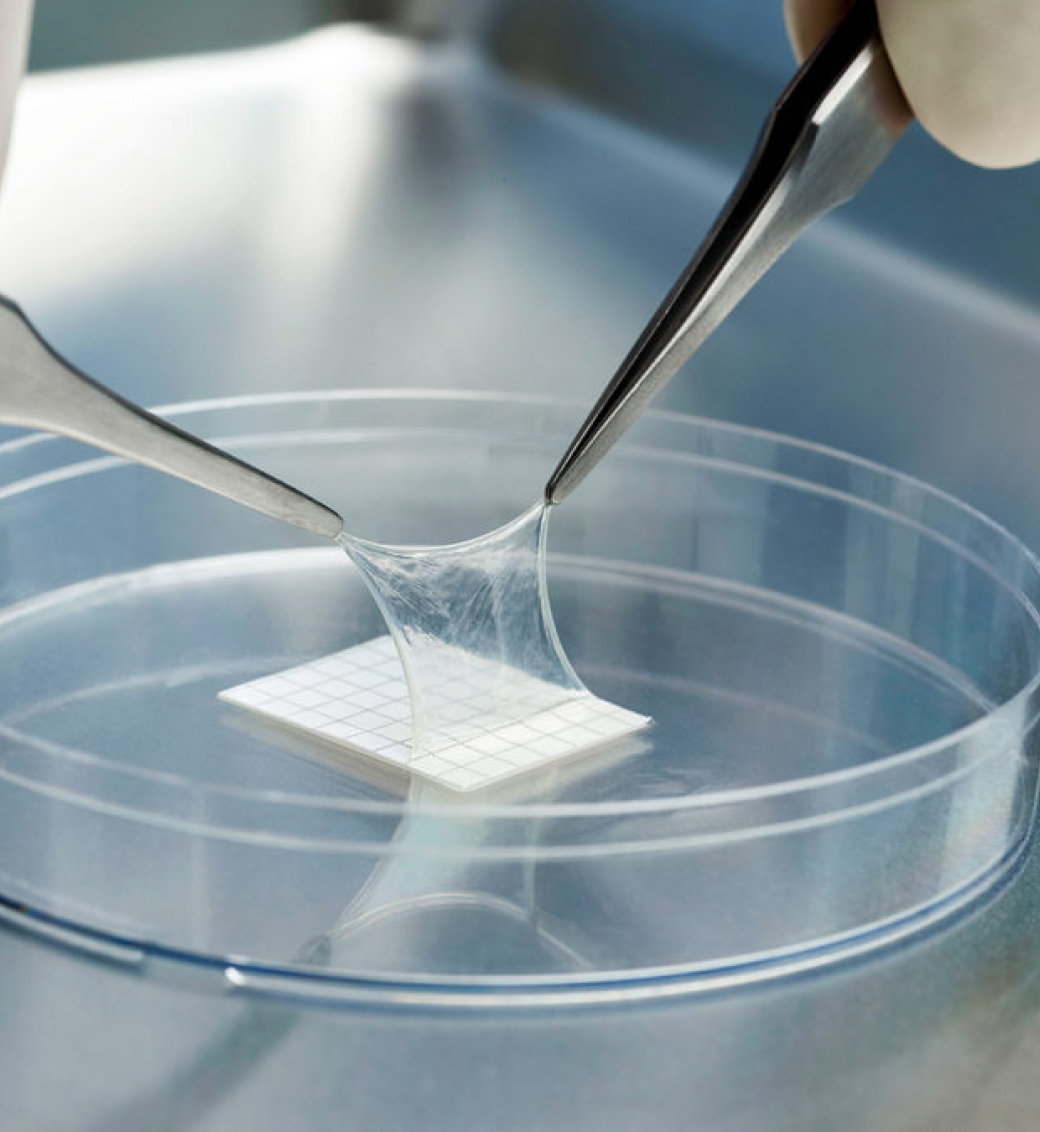
The BioTissue comprehensive family of human birth tissue allografts provides Mother Nature’s most natural gift to help expedite regenerative healing across a wide range of specialties as the adjunct for acute and chronic wound applications by:
- Facilitating wound healing
- Managing discomfort
- Managing adhesions
- Expediting functional recovery while reducing the cost of care1-3

Downloadable Resources
Downloadable Resources