
Surgical
Neox 1K
When Cost of Care Matters.
Neox® 1K is a cryopreserved ultra-thick human amniotic membrane allograft that can help expedite healing with fewer applications, reducing the cost of care.1,2 Neox can be used as an adjunct across a range of acute and chronic wounds.
Technology
Preserving as Much of Nature as Possible
The BioTissue CryoTek® cryopreservation process is the only tissue processing method shown to produce a matrix comparable to the native tissue.3,4
In conventional heat dehydration processing, critical biological components—including the majority of HC-HA/PTX3 naturally found in birth tissue—are degraded, which may limit the tissue’s healing capabilities.

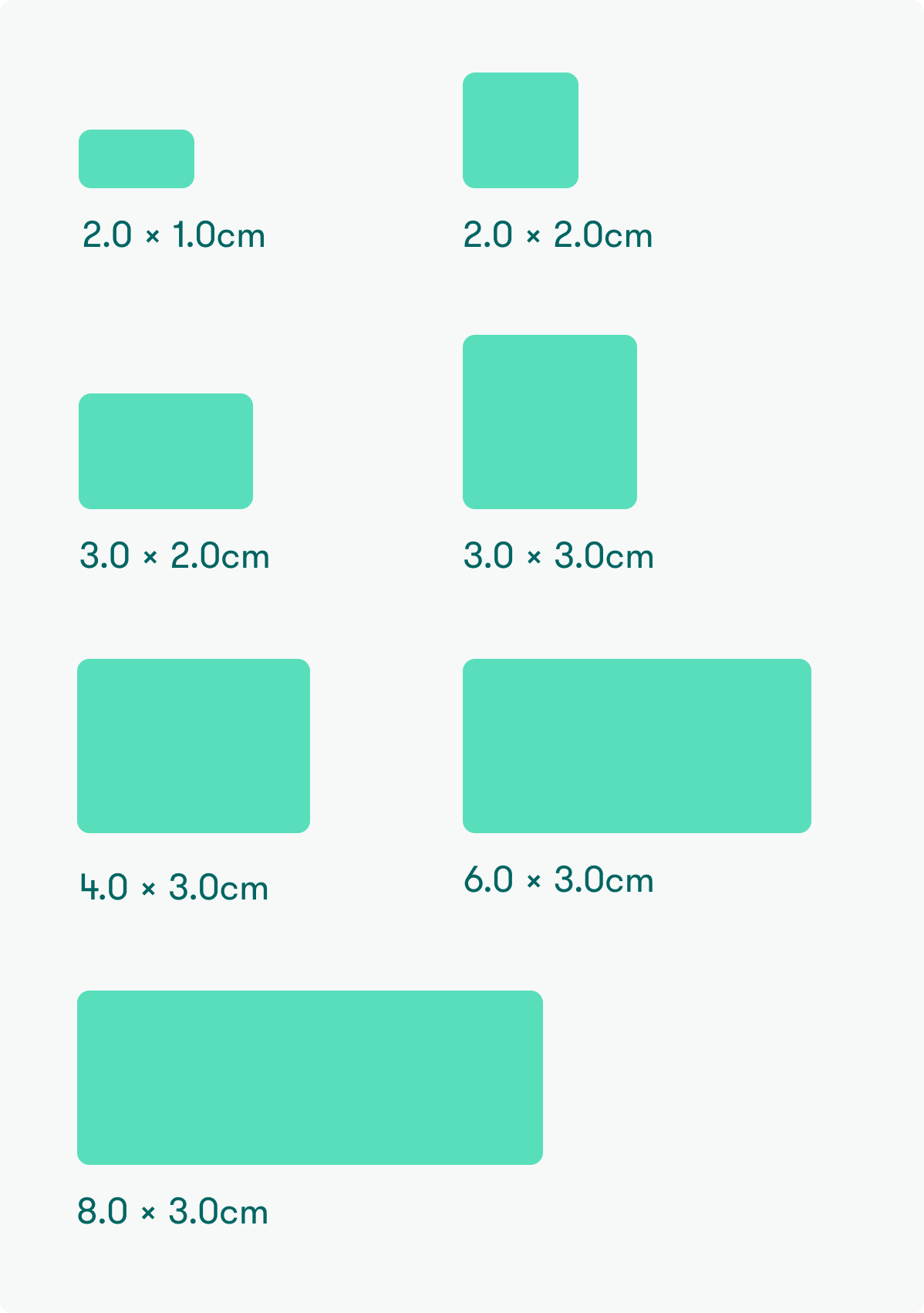
Available Sizes
NX-10-2010 (2.0 x 1.0 cm)
NX-10-2020 (2.0 x 2.0 cm)
NX-10-3020 (3.0 x 2.0 cm)
NX-10-3030 (3.0 x 3.0 cm)
NX-10-4030 (4.0 x 3.0 cm)
NX-10-6030 (6.0 x 3.0 cm)
NX-10-8030 (8.0 x 3.0 cm)
For a wide array of wound applications:
- Diabetic Foot Ulcers
- Chronic Wounds
- Venous Leg Ulcers
- Arterial Ulcers
- Pressure Ulcers
- Wound Dehiscence
- Burns
Location & Temperature
-80°C → 4°C (-112°F → 39.2°F)
Example: ultra-low temperature freezer, standard freezer, or standard refrigerator
Shelf Life
Within the expiration date printed on product packaging (2 years from date of manufacture)
The Neox allograft requires minimal preparation. No rehydration or thawing.
Neox 1K exposed to controlled room temperature (20°C to 25°C, 68°F to 77°F) for up to 6 hours may be returned to cold temperature storage in accordance with the Storage section as long as the packaging remains unopened and intact.
For Neox reimbursement information, visit the Reimbursement page.
For case studies, register for the Physician Portal.
BioTissue Surgical Customer Support:
Call us Monday – Friday: 9:00 a.m. to 7:00 p.m. Eastern Standard Time.
Email: [email protected]
Call: (888) 709-2140
Fax: (770) 874-5563
For more information, visit our Ordering page.
Download Neox 1K Product Information
To learn more about Neox, fill out the details below:
Neox
The time is now to achieve a new standard of care. Together we can make a difference in complex wound management.




